Trigeminal Neuralgia
Trigeminal Neuralgia Treatment Center of Virginia
A Patient’s Guide to Understanding of TN
A GUIDE TO USING THIS BOOKLET
This booklet is designed to give you the patient a brief education about trigeminal neuralgia and the treatments offered through Dr. K. Singh Sahni. We have tried to explain difficult terms and concepts in lay terms. For instance, you will find unfamiliar medical terms in bold italics explained within the text and in the glossary that follows. Of course, this information is by no means exhaustive or all-inclusive, and you are encouraged to discuss any specific concerns or questions with your surgeon.
TRIGEMINAL NEURALGIA
Trigeminal Neuralgia (TN), also known as tic douloureux, has been described as one of the most painful human afflictions. It has been compared to severe toothache or even labor pain. The pain is usually sharp and shooting and is very episodic and intermittent. It involves the trigeminal nerve which provides sensation to the face, teeth, mouth and nose. In most but not all patients, symptoms can be triggered by touching the face, brushing the teeth, feeling a breeze of air, putting on makeup, shaving, or merely touching certain parts of the face.
There is no specific test that can identify trigeminal neuralgia, so the best method of diagnosis is to obtain a good history from the patient. About two percent of trigeminal neuralgia patients harbor a tumor or some other sort of mass compressing the trigeminal nerve. Some of the most common causes are believed to be:
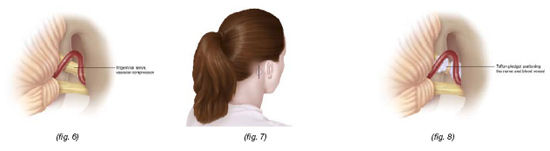
Vascular compression in which a blood vessel causes compression on the trigeminal nerve in the region very close to the brain stem called the root entry zone. (fig. 6)|
Multiple sclerosis (MS), While trigeminal neuralgia is usually found in patients over the age of 50, multiple sclerosis patients are usually younger than the average TN patient and may have bilateral (two sided) facial pain. Every young person with trigeminal neuralgia does not necessarily have MS.
A physician experienced in the management of trigeminal neuralgia can often make the appropriate diagnosis in a single interview.
The trigeminal nerve, also known as the fifth cranial nerve, has three branches:
1. Ophthalmic (around the eye);
2. Maxillary (around the upper jaw);
3. Mandibular (around the lower jaw).
The pain may be limited to one or more of these branches. In fact, many categorize the pain as atypical if it spreads beyond the distribution of the trigeminal nerve. For example, pain going down to the neck, shoulder, on top of or behind the head would not be coming from the trigeminal nerve. Trigeminal neuralgia involves attacks of severe pain on the affected side of the face and is rarely bilateral. The sharp attack may last just for a few seconds, but in advanced cases these attacks could last much longer. As mentioned above, the exception to this rule is the multiple sclerosis patient who may suffer from bilateral facial pain.
TREATMENT OPTIONS
Medications
In general, the first line of treatment for trigeminal neuralgia is medical. Anticonvulsants are frequently used for medical treatment of trigeminal neuralgia. For the majority of patients, these medications are quite effective.
Medical treatment with anticonvulsants must be tailored to the patient’s medical condition, age and general medical status including kidney and liver function since many of these medications may have effects with long-term use on kidney and liver function if they are not closely monitored. Usually the prescribing physician will closely monitor the dosage and obtain kidney and liver functions tests as well as blood counts for as long as these medications are taken.
Surgery
Patients unable to tolerate the medications or whose pain has become refractory (resistant to treatment) are then referred to a neurosurgeon with special interest and experience with trigeminal neuralgia. The three primary surgical options for the treatment of trigeminal neuralgia are:
Trigeminal Glycerol Rhizolysis (TGR)
Microvascular Decompression (MVD)
Gamma Knife (GK)
Trigeminal Glycerol Rhizolysis (TGR)
A procedure done in the hospital operat-ing room under monitored anesthesia. The anesthesiologist will utilize appropriate medications to decrease anxiety and help with sedation. General anesthesia (being put to sleep) is usually not necessary; however, intravenous medications are given so that you will be very relaxed and sleepy. In the majority of cases, you will not even remember the procedure. This is called IV sedation.
After being properly sedated, you will be placed on the operating table and a special x-ray device will be used to help the neurosurgeon insert the needle. The needle is advanced until it reaches a small pocket of fluid surrounding the trigeminal nerve (fig. 1). A special contrast (dye) is then injected which can be easily seen on the x-ray, and this determines the volume of fluid around the trigeminal nerve (fig. 2). In this way, the surgeon can calculate the exact amount of glycerol that needs to be given. This is an important part of the procedure and we find it an extremely important part of the process to avoid giving an overdose of the glycerol. Once the glycerol is measured and injected into this pocket, the needle is removed.
During this part of the procedure, you will usually be sitting up in the operating room after which you are transferred to a stretcher in the same position, sitting with the chin flexed and the head turned to the side of the procedure. The nurse in the recovery room will help you remain in that position for the next two hours during which time you will be closely monitored for comfort, your pulse, blood pressure and breathing will be closely watched.
IMPORTANT REMINDERS ABOUT TRIGEMINAL GLYCEROL RHIZOLYSIS
Generally you will not be “put to sleep”, but you must have nothing to eat or drink after midnight on the night before the procedure. You may resume your usual diet after surgery.
The area around the needle will be numbed before insertion of the needle; therefore, you should let your doctor know if you have any pain.
There will be no incision made. A band-aid will be used to cover the area where the needle was inserted. The band-aid may be removed the day after the procedure.
If you are taking any blood thinners such as aspirin, Plavix, Coumadin or any other such medications, please inform your physician so that they can be withheld with appropriate approval from your primary care physicians prior to the procedure.
Patients can usually go home the same day or the day after the procedure with a follow-up appointment to be seen back in the office in three to four weeks.
If you are taking any anticonvulsants, you will probably stay on the medication as advised by your surgeon. The medication will probably be decreased on your first follow-up appointment. Generally about a month later you will gradually be taken off the medications.
Notify your surgeon immediately if you have severe headache, nausea, vomiting, neck stiffness or fever.
Results
Some patients are completely pain-free within twenty-four hours of the procedure while others can take as long as three to six weeks to gain complete relief.
TGR is the preferred surgical approach for elderly patients with some medical issues who are in such extreme distress that they need urgent and immediate relief.
Patients are forewarned that there is a small risk of potential complications including some loss of feeling or decreased sensation of the face. If there is any numbness along the cornea or eye, you must be extremely careful and see an eye doctor. Your surgeon will go over the details of other potential risks and benefits of each procedure.
Some patients may develop fever blisters after the injection which usually go away quickly and need only to be taken care of with good hygiene and appropriate medications if needed.
Gamma Knife
Gamma Knife treatment is done under the leadership of a neurosurgeon, a team of physicists – doctors specializing in radiation – and nurses. Gamma Knife was pioneered in Stockholm, Sweden by Professor Lars Leksell and has been in use for more than thirty-five years. It is actually not a knife at all but is a term used for 201 individual beams of focused radiation that all converge on a selected target. While each individual beam is not very effective, the combination of all the beams causes a biological and structural change in the targeted tissue. Trigeminal neuralgia is just one of the indications for Gamma Knife, which is also used for brain tumors.
Gamma Knife for trigeminal neuralgia is performed for patients who are not ideal candidates for open surgery, such as patients on blood thinners or who have other known cardiovascular problems and patients unable or unwilling to take anticonvulsants. Others prefer this treatment due to its relative less invasiveness. Gamma Knife treatment is a simple,
relatively painless and quite straight- forward process that consists of four steps:
- Attaching the head frame;
- Imaging with MRI or CT scan (for patients with pacemakers)
- Treatment planning; and
- Treatment
Prior to treatment, your surgeon will review the entire procedure with you and risks and benefits will be discussed in great depth. Ample opportunity will be given for any questions you may have. given for any questions you may have. Usually, no incisions, stitches or shaving of the head is necessary. You will be offered to tour the Gamma Knife facility, watch an instructional DVD and meet the nurses.
PROCEDURE
1. The Head Frame
Placement of the frame on the head of the patient is a very important part of the procedure (fig. 3). This frame allows the doctor to pinpoint the target area with extremely high accuracy. For trigeminal neuralgia patients, the target is usually in the vicinity of the root entry zone of the fifth cranial nerve. This is actually the area where the trigeminal nerve originates in the brain stem. The anesthesiologist will give a very light intravenous sedation so that the patient will not experience any major pain or discomfort. The majority of patients do not even remember this part of the procedure because of the IV sedation.
2. Imaging
You will then be taken for imaging in a wheelchair or on a stretcher. During this part of the procedure, most patients are awake and alert; however, patients who experience anxiety about the MRI or CT scan can be given further sedation so that the imaging can be carried out.
3. Treatment Planning
At this point, you and up to three visitors will be able to sit together in the pretreatment area while the surgeon and the rest of his team work on the treatment plan.
The process may take up to forty minutes. Family members accompanying the patient may feel free to bring reading or work materials with them. There is also a television and DVD player in the room for entertainment.
During treatment planning, data from the images is transferred to a special, highly sophisticated computer. Unlike gamma knife treatment for brain tumors in which the tumor is outlined, trigeminal neuralgia patients will have the nerve outlined in multiple imaging sequences.
Your neurosurgeon and the rest of the team will go through a quality assurance process and everyone will review and confirm the plan before embarking on the actual treatment.
4. Treatment
You will then be taken to the actual Gamma Knife Suite where you will be allowed to lie down in a comfortable position (fig. 5). The head frame is now attached to the automatic position system (APS). This is a very sophisticated computerized robotic system with high accuracy. At this point, you may move your arms and legs, but your head will actually be fixed. All of this will be explained by the nurses and doctors once inside the unit.
The treatment itself is silent, completely painless and lasts roughly 30 minutes. Patients can even bring their favorite CD so they can listen to their music during the treatment. Some prefer to sleep through the procedure, and in this case a mild sedative is given just before the procedure if needed. The treatment is completely monitored by the team via a camera in the treatment room. A nurse is also just outside the room who can see the treatment room on a video screen and communicate with the patient by microphone. Once the treatment is completed, you will be allowed to walk back to the patient suite accompanied by a nurse. The frame is removed, again with very minimal discomfort, and a dressing is placed. You will be given another half-hour or hour to completely recover depending on the amount of sedation. Once you have completely recovered and are ready to go home, you will be discharged. Gamma Knife is generally an outpatient procedure.
Important Reminders About Gamma Knife
1) Generally you will not be put to sleep, but you must have nothing to eat or drink after midnight on the night before the procedure. You may resume your usual diet after surgery.
2) If you are taking any blood thinners such as aspirin, Plavix, Coumadin or any
other such medications, please inform your physician so that they can be withheld with appropriate approval from your primary care physician prior to the procedure.
3) Keep pin sites clean with alcohol the day after the procedure.
4) You may shower the next day without restriction.
5) There may be some swelling around the pin sites to which ice can be applied.
6) Medications taken for trigeminal neuralgia may be continued as before.
Going Home and Results
While some experience immediate relief with gamma knife, the majority of patients take six to eight weeks to notice major improvement in the trigeminal neuralgia pain. As the pain decreases, you will be encouraged to gradually wean yourself off the medication after discussion with your physician.
Regular follow-up is very important, and you will be given an appointment to follow up in the office usually six to eight weeks after the procedure. The first follow-up scan will be done in about six months to view the radiographic effect of this treatment. If you are coming from out-of-town, it is important to obtain the MRI’s or have them sent to your neurosurgeon for his review.
It is very important to keep your follow-up appointments. If you do not come to these appointments and you cannot be located, we will have to consider your treatment a failure even if you are well. Please notify us of any address or phone number changes. We may want to contact you even after your regular follow-up visit to keep appropriate statistics about long-term results. Please consider sending us a yearly letter or postcard to let us know how you are doing.
Out-of-Town Patients
Gamma Knife Treatment for Trigeminal Neuralgia is usually done as an outpatient procedure, and patients do not need to be admitted to the hospital. For out-of-town patients, we have special discounted rates with area hotels for which information is available upon request.
MICROVASCULAR DECOMPRESSION
Microvascular Decompression (MVD), which is considered the most invasive form of surgical treatment for Trigeminal Neuralgia isalso the procedure with the highest success rate. Since this is an invasive procedure, it is reserved for a small subsection of patients. Patients who are in generally good health without major medical problems may be considered for Microvascular Decompression. Microvascular Decompression is also offered to patients who may have failed the less invasive procedures such as Trigeminal Glycerol Rhizolysis and Gamma Knife Treatment.
As mentioned in the introduction to this booklet, vascular compression of the Trigeminal Nerve or fifth cranial nerve is thought to be the culprit for this painful syndrome in a significant number of Trigeminal Neuralgia patients. Compression of the nerve is usually by a blood vessel although very rarely compression could also be from a tumor or some other vascular abnormality (fig. 6)
Preoperative Planning
Remember to inform your doctor if you have any specific allergies. If you are on aspirin, Coumadin, Plavix, or any other blood thinners, be sure that you have informed your doctor and discontinued these medications with appropriate approval for at least a few days prior to the operation. On the eve of your operation, make sure you have showered and shampooed your hair very thoroughly without applying any sort of spray, mousse, gel or any other such material. A small portion of hair behind the ear will have to be shaved for the operation, and it is best not to have applied any greasy or oily material and to have the hair in its cleanest, natural form for this. You will need to make a list of all the medications you have been taking at home to provide to your physician. You will have to sign a consent form for the operation which will include consent for a blood transfusion. It is extremely rare for blood to be used for these surgeries, but permission is obtained in case of an extremely unexpected emergency situation. You may discuss this matter with your surgeon ahead of time if you have any specific concerns about this matter.
You will be advised not to eat or drink after midnight, and it is best to stay on
a very light and liquid diet for the entire
day before the operation. Blood pressure medications should not be withheld, but no blood thinners such as aspirin, Plavix or Coumadin should be taken for a few days prior to the operation. If you are on blood pressure medications or other cardiac medications other than blood thinners, it is usually advisable to take this with a sip of water. Any herbal medications such as garlic pills, fish oil, etc., be sure to inform your surgeon. Most likely you will be asked to stop those for a few days before your operation as well.
The Surgical Procedure
Unlike the other procedures, Microvascular Decompression requires general anesthesia which means this is done in the operating room with you completely unconscious and the anesthesiologist monitoring you throughout the operation. A small incision will be made behind the ear (fig. 7) on the same side as the trigeminal neuralgia pain. The incision is carried down through the skull and a very small hole is made as a window to approach this blood vessel. The covering of the brain, called the dura, is opened, and medications are usually given to allow the brain to relax so that the surgeon can work through a very small angle under microscopic magnification to expose the nerve. Once the nerve is exposed and particularly when its entrance to the brain stem is seen, a careful inspection is done for vascular compression. After detecting the vascular compression, the surgeon will elevate the blood vessel off of the nerve and place pledgelets of Teflon (fig. 8). The Teflon material is synthetic and is easily placed between the nerve and the vessel. This creates a partition between the nerve and the vessel so that the vessel no longer pulsates on the brain stem. Closure is done by suturing the dura and placing a synthetic material to cover the hole made in the bone. Upon completion, there is no defect in the bone and the incision will heal very nicely.
Once the surgery is complete, you will be transferred to the recovery room. The surgeon will then explain the results to your family in the waiting room and you will be transferred to the Neuroscience Intensive Care Unit (NICU).
Usually you will spend one night in the Neuroscience Intensive Care Unit with mobilization the following day out of ICU to a regular private room. On the first day after surgery, you will usually be allowed to get out of bed and have breakfast. The dressing will not be changed for three days. On the second or third day, the patient is discharged after dressing change.
Results
The results of Microvascular Decompression are usually very good, and there is usually a much lower recurrence rate than with other procedures. However, this is a major surgical intervention, and the potential for complications is also much higher compared to less invasive procedures of Trigeminal Glycerol Rhizolysis and Gamma Knife Treatment. Since this is an open operation, it does carry the potential complications that come with general anesthesia. At the same time, other potential risks of open procedure such as hemorrhage, stroke, loss of function of certain cranial nerves – specifically loss of hearing in a very small percentage of patients – must be given consideration.
In experienced hands, this surgery has very good results, but even in the best of hands major complications can occur, and details should be thoroughly discussed with your surgeon. Whenever Microvascular Decompression is offered, your surgeon will sit down with
you and your family members and go over the entire protocol of the operation with thorough discussion of the risks and benefits. Ample opportunity will be provided for you and your family to ask and receive satisfactory answers to questions.
Discharge Planning
Once you are discharged, you will be advised to keep your head elevated on two or three pillows for at least two to three weeks. You will usually be instructed not to get your incision wet until return to the surgeon’s office for removal of the stitches and dressing change. During the first seven to ten days, you must refrain from any strenuous activities such as lifting, bending or for that matter even driving. After ten days and having seen the surgeon in the office for the first follow-up visit, you are usually allowed to return to normal activities.
We usually instruct patients to stay very active after the operation and encourage you to start moving as soon as you are stable and regain complete balance. It is very important to keep in mind that while the patient is in the bed and not ambulating, the blood can pool in the leg and lead to blood clots in the legs, which can be very dangerous. To prevent this during the operation and your stay in the intensive care unit, special stockings are used which cause intermittent massage and compression of the legs. This helps to prevent the formation of any blood clots in the leg. Once you are transferred to a regular room and after you are discharged home, you should continue to wear TED hose stockings until you are very active with ambulation and no longer need the elastic hose. It is very important for smokers to quit smoking several days before the operation. Deep breathing and gentle coughing exercises after surgery are also very important to keep your lungs moving and prevent pneumonia. Usually a nurse and the respiratory therapist will help to educate you on specific exercises during your hospital stay. Elderly patients and smokers are especially encouraged to
continue these exercises at home.
If you notice any leakage of fluid through the nose or back of the throat, you should immediately alert your surgeon, as this could be a sign of spinal fluid leakage from the surgery. If you experience fever, headache, nausea, vomiting, neck stiffness or any such problems, the surgeon should also be promptly informed. Most patients are taken off of anticonvulsants rather quickly after this operation unless you have been on the medication for a very long time in which case you will be gradually tapered off.
Final Decision
Dr. K. Singh Sahni spends a lot of time discussing each individual procedure with his patients and family members.
The final decision to select the surgical procedure is made by the patient while Dr. Sahni helps them with this process.
You should feel comfortable asking any questions during your consultation with Dr. Sahni. He has a lot of patience and compassion for his TN patients.
About the Surgeon
K. Singh Sahni, MD, FACS is a distinguished neurosurgeon with a special interest in the treatment of trigeminal neuralgia. Over the last twenty years, he has treated close to 2,000 patients who suffer with facial pain syndromes. While there are a number of physicians who may offer one or the other preferred methods of treatment for trigeminal neuralgia, as one who subspecializes in this disease Dr. Sahni has expertise in all methods of treatment, surgical and nonsurgical. This enables him to tailor each patient’s treatment based on the patient’s age, general medical condition and overall manifestation of pain. All of this affords the best-case scenario for the trigeminal neuralgia patient of having the opportunity to work with a neurosurgeon who is able to offer all treatment options at the same facility with a single physician without bias toward a specific procedure. Dr. Sahni is a board certified Neurosurgeon. He is the Medical director of Gamma Knife Unit. He obtained his GK training in Stockholm, Sweden. Dr. Sahni has been performing TGR (Glycerol injections) and MVD (Microvasular Decompression) for over twenty years.
Glossary of unfamiliar terms
Aplastic anemia: Low white blood cell count caused by decreased bone marrow function.
Bilateral: Two-sided.
Dura: The covering of the brain.
Fifth cranial nerve: Cranial nerve that serves the face, teeth, mouth and nose. Same as trigeminal nerve.
GK: Gamma Knife
Intractable: Resistant to cure, relief or control.
Mandibular: Related to the lower jaw.
Maxillary: Related to the upper jaw.
MVD: Microvascular Decompression
Ophthalmic: Related to the eye.
Refractory: Resistant to treatment.
Root entry zone: The region very close to the brain stem, especially where the trigeminal nerve originates.
TGR: Trigeminal Glyerol Rhizolysis
Tic douloureus: Painful condition characterized by severe, excruciating, episodic face pain. Same as trigeminal neuralgia.
Trigeminal nerve: Cranial nerve that serves the face, teeth, mouth and nose.